If you’ve spent even five minutes in a pediatrician’s waiting room over the last decade, you’ve probably noticed something that wasn’t nearly as common years ago: babies wearing small, custom-fitted helmets. Some parents look reassured. Others look worried. A few look overwhelmed, Googling frantically on their phones.
That moment—standing between confusion and clarity—is exactly why cranial technology has become such an important conversation.
Cranial technology sits at the intersection of pediatric healthcare, biomedical engineering, and real-life parenting decisions. It addresses skull shape irregularities in infants, conditions that are more visible today than ever before. And while the technology itself has advanced rapidly, the information parents receive is often fragmented, oversimplified, or emotionally charged.
This guide is written for parents, clinicians, healthcare writers, and anyone who wants a grounded, experience-based understanding of cranial technology—without the hype, fear-mongering, or shallow explanations.
You’ll learn what cranial technology actually is, how it works in the real world, when it’s appropriate, what tools and systems professionals rely on, common mistakes families make, and how to approach decisions with confidence instead of panic.
Most importantly, this article focuses on practical clarity. No fluff. No scare tactics. Just informed, balanced insight from a real-world perspective.
What Is Cranial Technology? A Clear, Human Explanation From Basics to Advanced
At its core, cranial technology refers to medical systems and processes designed to assess, monitor, and guide the growth of an infant’s skull during early development. The most common application involves cranial remolding orthoses—custom helmets designed to gently correct head shape asymmetries.
To understand why this exists, imagine the infant skull like a soft, partially assembled puzzle. The bones haven’t fused yet. That flexibility is essential for brain growth, but it also means external forces—sleeping position, muscle tightness, or time spent on one side—can influence shape.
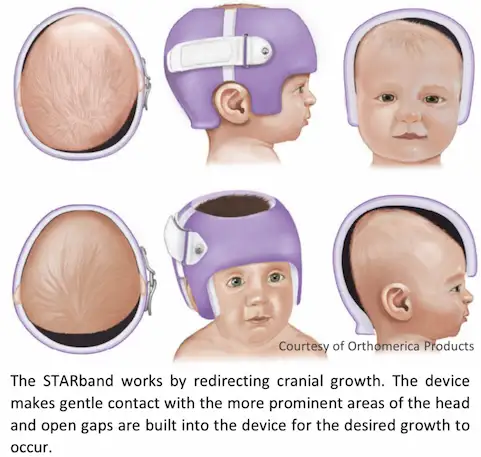
Cranial technology doesn’t “push” the skull into place. That’s a common myth. Instead, it works by providing space where growth is needed and limiting it where growth is excessive. The brain continues to grow naturally; the helmet simply guides that growth toward symmetry.
Modern cranial technology relies on several components working together:
First, advanced scanning systems—often laser-based or optical—create a precise 3D map of an infant’s head. These scans are fast, non-invasive, and far more accurate than old-school tape measurements.
Second, proprietary modeling software analyzes asymmetries, growth vectors, and expected changes over time. This is where experience matters. Technology provides data, but trained clinicians interpret it.
Third, custom-fabricated cranial orthoses are created using medical-grade materials designed for comfort, hygiene, and continuous wear.
Companies like Cranial Technologies pioneered much of this integrated approach, combining diagnostics, design, and follow-up care into a single clinical workflow. Their best-known product, the DOC Band, became almost synonymous with helmet therapy in many regions.
The important takeaway is this: cranial technology is not a cosmetic shortcut. It’s a structured medical intervention built around growth science, biomechanics, and data-driven adjustments.
Who Cranial Technology Is For: Conditions, Candidates, and Real-Life Scenarios
One of the biggest misunderstandings around cranial technology is that it’s for “any baby with a slightly flat head.” That’s not accurate, and it’s where anxiety often creeps in.
Cranial technology is most commonly used to address positional plagiocephaly, brachycephaly, and scaphocephaly—conditions related to skull shape rather than brain development. These conditions have become more visible since the widespread adoption of safe sleep practices, which encourage infants to sleep on their backs.
Here’s what that looks like in real life.
A baby who consistently favors turning their head to one side may develop flattening on that side of the skull. Over time, facial asymmetry can appear—one ear slightly forward, one cheek fuller than the other. Parents often notice it in photos before they see it in the mirror.
Cranial technology is typically recommended when:
Conservative measures like repositioning and physical therapy haven’t produced sufficient improvement
Asymmetry measurements cross clinical thresholds
The baby is within an optimal age window, usually between 4 and 12 months
Timing matters because skull growth is fastest in the first year. Cranial technology works with that growth curve, not against it.
The families who benefit most are those who want structured guidance rather than guesswork. Instead of constantly wondering whether things are improving, they receive measurable data at each visit.
Benefits of Cranial Technology: Real Outcomes Beyond Appearance
It’s easy to assume the primary benefit of cranial technology is cosmetic. That assumption misses the bigger picture.
Yes, head shape symmetry improves. But the real value lies in predictability, peace of mind, and long-term functional considerations.
Parents often describe the “before” phase as mentally exhausting. Constant repositioning. Worrying during sleep. Questioning every photo. After cranial technology is introduced, there’s a clear plan.
Clinically, benefits include:
Objective measurement of progress instead of subjective observation
Reduced facial asymmetry as skull alignment improves
Decreased risk of secondary issues related to severe asymmetry
From a practical standpoint, families often report improved routines. Babies adapt to helmets far faster than adults expect. Most wear them 23 hours a day with minimal disruption to feeding, sleeping, or play.
For clinicians, cranial technology creates standardized care pathways. Instead of relying solely on visual judgment, they can track outcomes over time and adjust treatment precisely.
The technology doesn’t replace expertise—it amplifies it.
A Step-by-Step Look at How Cranial Technology Works in Practice
Understanding the process removes much of the fear. Here’s how cranial technology typically unfolds from start to finish.
The journey begins with an evaluation. This includes a physical exam and a digital scan. The scan takes seconds and produces a high-resolution 3D model of the infant’s head.
Next comes data analysis. Clinicians assess asymmetry indices, growth potential, and age-related factors. This is where experience matters most. Numbers alone don’t make decisions—context does.
If cranial technology is recommended, a custom orthosis is designed. Using CAD/CAM systems, technicians create a helmet that fits precisely while leaving room in targeted growth areas.
Once fitted, follow-up becomes the backbone of success. Regular appointments ensure:
The helmet remains comfortable
Growth is tracking as expected
Adjustments are made as the skull changes
This isn’t a “set it and forget it” process. The technology evolves with the child.
Treatment duration varies but typically ranges from 3 to 6 months, depending on age and severity. Consistency is key. The helmet only works when worn as prescribed.
Tools and Systems Behind Modern Cranial Technology


Not all cranial technology is created equal. The difference between average and excellent outcomes often comes down to tools and clinical infrastructure.
High-quality programs rely on:
Non-invasive 3D scanning systems instead of plaster molds
Advanced modeling software for growth prediction
Medical-grade materials optimized for airflow and hygiene
Large providers like Cranial Technologies invest heavily in proprietary systems, while smaller clinics may partner with third-party labs.
Free or low-cost alternatives, such as repositioning apps or head-shape pillows, can help in mild cases but lack the precision of clinical cranial technology.
From an expert perspective, the best system is one that combines technology with continuity of care. Tools don’t replace follow-up. They support it.
Common Mistakes Parents Make—and How to Avoid Them
The most common mistake isn’t choosing cranial technology. It’s waiting too long out of fear or misinformation.
Parents often hear, “They’ll grow out of it.” Sometimes that’s true. Sometimes it isn’t. The risk lies in assuming improvement without measurement.
Another frequent issue is inconsistent wear. A helmet worn 18 hours a day instead of 23 significantly reduces effectiveness. Not because the technology fails, but because growth doesn’t pause when the helmet is off.
Some families also focus too much on online anecdotes. Every baby is different. What matters is your child’s data, not someone else’s timeline.
The fix is straightforward:
Get an objective evaluation early
Follow evidence-based recommendations
Commit fully if you begin treatment
Cranial technology rewards consistency and informed decisions.
The Future of Cranial Technology: Where Innovation Is Heading
Cranial technology continues to evolve. AI-assisted modeling, remote monitoring, and lighter materials are already reshaping the field.
We’re seeing early movement toward predictive growth simulations, allowing clinicians to model multiple treatment scenarios before fabrication. Telehealth check-ins may reduce visit frequency without sacrificing accuracy.
What won’t change is the need for human expertise. Technology supports judgment—it doesn’t replace it.
Conclusion: Making Confident Decisions With Cranial Technology
Cranial technology isn’t about perfection. It’s about guidance during a brief, critical window of development.
When used appropriately, it offers clarity where uncertainty once ruled. It turns guesswork into measurable progress and replaces anxiety with a plan.
If you’re considering cranial technology, the best next step is an informed evaluation. Ask questions. Review data. Choose providers who prioritize education over pressure.
The technology works best when paired with understanding—and now, you have that foundation.
FAQs
Is cranial technology safe for infants?
Yes. Modern cranial technology is non-invasive and designed to work with natural growth.
Does helmet therapy hurt babies?
No. Properly fitted helmets apply no pressure and are generally well tolerated.
When is the best age to start cranial technology?
Typically between 4 and 8 months, when skull growth is most rapid.
How long does treatment usually last?
Most treatments last 3 to 6 months, depending on severity and age.
Can repositioning replace cranial technology?
In mild cases, yes. Moderate to severe cases often require clinical intervention.
Adrian Cole is a technology researcher and AI content specialist with more than seven years of experience studying automation, machine learning models, and digital innovation. He has worked with multiple tech startups as a consultant, helping them adopt smarter tools and build data-driven systems. Adrian writes simple, clear, and practical explanations of complex tech topics so readers can easily understand the future of AI.